
Endoscopic Mucosal Resection (EMR) and Endoscopic Submucosal Dissection (ESD) are advanced endoscopic techniques designed to remove precancerous lesions, polyps, and early-stage cancers from the gastrointestinal (GI) tract without the need for major surgery. Both procedures are minimally invasive alternatives to traditional surgery and play a vital role in the early management of gastrointestinal cancers.
1. EMR is used for the removal of abnormal or early cancerous tissue limited to the mucosal layer (the innermost lining of the GI tract).
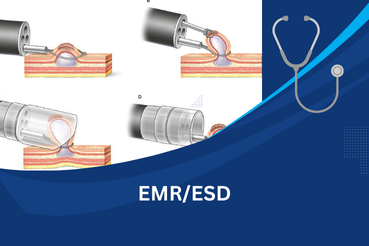
2. During EMR, a flexible endoscope is inserted into the GI tract, and fluid is injected beneath the lesion to lift it away from the deeper layers. The lesion is then snared and removed with the help of an electrical current.
3. It is particularly useful for polyps, small tumors, and precancerous growths in the esophagus, stomach, colon, and rectum.
1. ESD is a more advanced technique used when lesions are larger, flat, or deeply embedded in the submucosal layer.
2. In ESD, after lifting the lesion, the doctor carefully dissects through the submucosal layer using special endoscopic knives, allowing en bloc removal (removing the entire lesion in one piece).
3. This ensures complete removal of larger or high-risk lesions and reduces the chances of recurrence compared to EMR.
4. ESD is commonly performed in the esophagus, stomach, and colon, especially for early cancers.
EMR is used for removing small, superficial lesions from the GI tract and is relatively quick. ESD, on the other hand, is designed for larger or deeper lesions and allows removal of the entire growth in one piece (en bloc), reducing recurrence but requiring more time and expertise.
No, patients do not feel pain during the procedure because it is performed under sedation or anesthesia. Afterward, mild discomfort, bloating, or sore throat may occur, but these usually resolve quickly.
The most common causes include viral infections (like hepatitis A, B, and C), excessive alcohol use, obesity (leading to non-alcoholic fatty liver disease), genetic conditions, autoimmune disorders, and long-term use of certain medications.
Both procedures are generally safe, but possible risks include bleeding, perforation (small tear in the intestinal wall), infection, or recurrence of the lesion. These risks are uncommon and can usually be managed effectively by the medical team.
Most patients can return home the same or next day. A short hospital stay may be required for observation, especially after ESD. Normal activities can usually be resumed within a few days, but the doctor may recommend a soft diet and follow-up endoscopy to ensure complete healing.